Knee Symptoms
The knee is the largest joint in the human body and its mechanics are extremely complicated. It is a “pivotal hinge joint”, which permits flexion and extension as well as some internal and external rotation. As knee supports almost the whole weight of the body, it is vulnerable to both acute injury and the development of osteoarthritis.
Covered on this page:
Knee Pain
Pain is by far the commonest symptom presenting to the knee clinic. The pain may be characterised by different features:- Gradual or sudden (acute) onset
- Constant or Intermittent
- Activity or rest related
- Sharp & stabbing or aching and burning
- General or localized
Knee Swelling or “Effusion”
It is normal for the knee to contain a small amount of yellowish liquid or “synovial fluid”. The normal volume (3 to 5mls) of fluid does not cause visible swelling. This complex fluid plays an essential role in lubricating the joint and provides nourishment to the cartilage surfaces covering the bone. The synovial lining of the knee often produces excess amounts of fluid in response to inflammation or direct injury. This leads to swelling (“an effusion”) and a tightness sensation within the joint. If the swelling gets tense the range of movement in the knee becomes restricted. If the knee sustains a direct injury it may fill with blood (termed a “Haemarthrosis”). A rapidly forming haemarthrosis (minutes to a few hours) may be associated with a ligament tear or an underlying fracture. Classically the haemarthrosis associated with an acute meniscal tear develops over many hours. Occasionally an acute haemarthrosis may be drained with a needle and syringe to make the knee more comfortable.Knee Instability
Often patients present to the knee clinic with symptoms of instability or “giving way” of the knee. This unpleasant sensation may occur as a result of damage to supporting structures (“true instability”) or as a “reflex” type response to a sudden pain causing muscle weakness. Occasionally this giving way may cause the knee to buckle completely leading to falls. Patients with pain arising from their patella often describe painful giving way symptoms when walking down stairs or slopes. Following an anterior cruciate ligament (ACL) injury patients often describe the knee giving way and buckling when they twist or change direction. It is common for them to”loose trust” in the knee – particularly during exercise or walking on uneven ground.Knees Locking and Catching
Locking symptoms can occur in the knee if loose fragments of cartilage or bone get caught in the mechanism of the joint. The classical presentation of a “locked knee” occurs following a period of kneeling or crouching followed by an inability to straighten the knee. Usually this is due to a tear in the shock absorbing meniscal cartilage “flipping” into the joint. Often the knee can be unlocked by shaking or wiggling the leg until the loose fragment moves back into place – often with a relieving “clunk”!. Occasionally catching and locking symptoms arise if a damaged and roughened area develops in the smooth articular cartilage on the joint surface – this is particularly common if arthritis develops behind the patella.Knee Stiffness
Stiffness is a common symptom of knee arthritis and following knee injury. After an acute (sporting type) injury the joint will typically feel stiff and “tight” for six weeks and then begin to loosen up as the swelling resolves. Gentle range of movement exercises, icing, compression bandaging and anti-inflammatory medications can help to settle this problem. Stiffness within the knee is very common in arthritis. As the joint surface wears and the ligaments around the knee tighten the stiffness tends to worsen. Eventually the range of movement reduces as full extension and flexion are no longer possible. Gentle stretching exercises and help from a physiotherapist can often help to reduce this problem.Knee Weakness
Muscle weakness is an inevitable consequence of any serious knee problem. Pain and mechanical instability prevent the normal use of the joint which is followed by shrinking (atrophy) of the surrounding muscles. Muscle weakness can lead the knee to feel vulnerable and unstable. It usually takes many months of hard work to restore the muscles to full power and function following knee injuries and more major knee surgery. Physiotherapists can often help speed up this rehabilitation process.Meniscal Problems
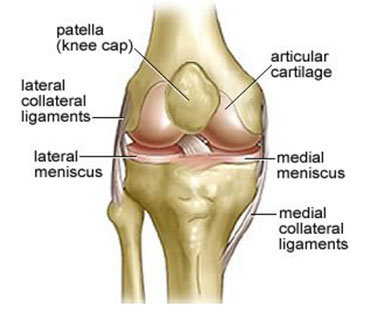
What are the menisci?
The menisci are crescent shaped cartilage structures separating the ends of the femur and tibia inside the knee. There are two menisci in each knee – one medially and one laterally. The menisci have a number of important functions:- They help share the load as forces pass through the joint
- They act as shock absorbers
- They help the nutrition and lubrication of the smooth articular cartilage
- They help stabilise the knee – especially if supporting ligaments have been damaged
How do meniscal tears occur?
There are two main types of meniscal tear – acute (traumatic) tears and degenerative (wear and tear) tears.
Acute tears most commonly occur in younger patients and often present following sporting or work related injuries. Classically the injury occurs whilst the knee is loaded followed by a twisting and flexing motion. Typically a sudden pain develops at the area of the meniscal tear followed by swelling over a few hours.
Degenerative tears tend to occur in an older population. Over time the menisci become less flexible and rather more friable and susceptible to damage from less traumatic injuries. Classically these tears present with a more insidious onset, with symptoms of intermittent pain, swelling and occasional catching.
What is the treatment for a meniscal tear?
Some of the symptoms of meniscal tear include:
Knee pain – usually on the inside or outside of the joint
Locking – the knee may intermittently lock and catch as the loose meniscal fragments get caught in the mechanics of the joint
Swelling – this may occur rapidly in an acute tear or be intermittent with degenerative tears
Lumps or “loose bodies” may be felt on the inside or outside of the joint if large fragments of meniscal tissue flip out of place
What are the symptoms of meniscal tear?
Some patients – particularly those with degenerative tears, respond well to conservative treatment with a period of rest and anti-inflammatory tablets followed by physiotherapy. If the symptoms from the tear are minor and not intrusive many patients choose to leave things as they are.
In cases where an acute tear has occurred, the knee is locked or where symptoms are more severe and have not responded to conservative management then surgery is often helpful. The vast majority of meniscal surgery is now performed arthroscopically as a day case procedure.
Meniscal repair
In some cases the tear in the meniscus may be amenable to repair with sutures. This is more likely to be the case in acute tears in younger patients. Following arthroscopic meniscal repair a knee brace is usually worn for six weeks to prevent excessive knee flexion. Impact loading, twisting and sporting activities should be avoided for 3 months to give the best chance of healing.
Success rates for meniscal repair are in the range of 60 to 90% depending upon the size, location, timing of the repair and concomitant injuries within the knee.
Meniscal resection
The majority of meniscal tears are not amenable to repair. In this situation the tear and any unstable cartilage is trimmed away. This helps to prevent further extension of the tear, improves catching symptoms and reduces pain caused by the tear irritating the sensitive synovial lining of the knee.
Cartilage Problems
What is articular cartilage?
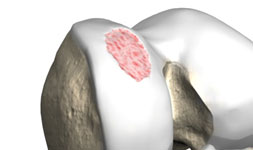
Articular (Hyaline) cartilage is the smooth, tough, white cartilage that covers the end of bones when they come together to form joints. The smooth cartilage allows joints to glide smoothly without catching. When the cartilage is lubricated with joint (synovial) fluid the friction between the bone ends is negligible. The cartilage itself has no nerve or blood supply, relying on the surrounding joint fluid and underlying bone for nutrition.What is cartilage damage?
Articular cartilage may become damaged by trauma or may become worn over time. Because of the lack of blood supply the cartilage has poor healing properties. This may lead to roughening of the joint surface and decline in joint function. Occasionally the underlying bone may become exposed, triggering painful arthritis symptoms within the joint.
What are the symptoms of articular cartilage damage?
The symptoms of articular cartilage damage depend upon the site and size of the injury. Small areas of cartilage loss may be completely asymptomatic. As the injured area becomes more extensive it is common for patients to develop catching or locking symptoms. If bone becomes exposed below the cartilage then the joint often becomes painful. If large areas of bone are exposed then osteoarthritis symptoms develop with pain, stiffness and swelling of the joint.
What is the treatment for articular cartilage damage?
The treatment for articular cartilage damage depends upon the symptoms and size of the problem. If conservative treatment has not helped then different surgical options may be considered.
Smaller, more localised areas of injury may be helped with restorative procedures to try and regenerate new cartilage to fill the damaged area. These types of procedures tend to work better in younger patients with more acute injuries. Large areas of injury and areas of arthritis are less likely to benefit from this type of surgery. Often this type of surgery can be performed arthroscopically or through small incisions around the joint.
The more common procedures for cartilage restoration include:
- Microfracture
- Autologous Membrane Induced Chondrogenesis (AMIC)
- Autologous Chondrocyte Implantation (ACI)
More extensive areas of cartilage loss (especially with areas of bone rubbing against bone), are not amenable to cartilage regeneration surgery. Joint replacement surgery may often be required in this situation. This may involve either partial or total joint replacement with metal, plastic or ceramic components.
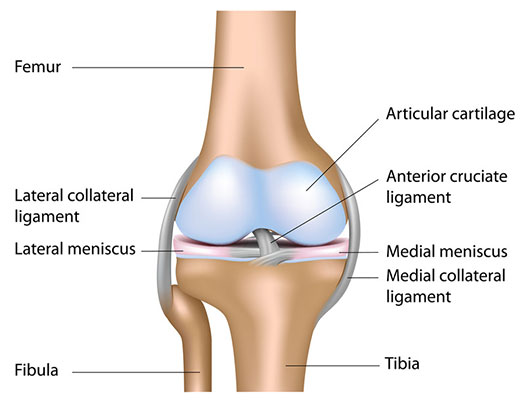
What are ligaments?
Ligaments are strong, flexible, fibrous structures that connect bones to other bones. Articular ligaments pass inside or around joints and provide strength and stability. Ligaments are made from collagen connective tissue. In some people the connective tissue may stretch more than others leading to joint laxity and the term “double-jointed” being used. Extreme laxity may lead to problems with joint dislocations or pain symptoms.
How are ligaments damaged?
Ligaments may become damaged when excessive forces pass around or across the joint. The ligament may tear in half (intra-substance tear) or be pulled from their attachments to bone (avulsions). Most commonly this type of injury occurs on the sports field but may be caused by any significant trauma. The ligament tear or avulsion may be partial or complete leading to varying levels of symptoms and joint laxity.
What are the symptoms of ligament damage?
Ligament tears tend to be acutely painful and often a “snap or pop” may be heard or felt as the ligament breaks. Usually the tear is associated with significant swelling and bruising as blood vessels often run within the ligament. Usually the swelling leads to stiffness and a restriction in the range of joint movement.
As the swelling within the joint subsides and the range of movement returns symptoms of instability may develop. This is often described as the joint feeling vulnerable during particular activities or may present as “giving-way” and collapse of the joint.
Common Knee Ligament Injuries
Anterior Cruciate Ligament Injuries (ACL)
The Anterior Cruciate Ligament (ACL) is a major stabilising ligament in the centre of the knee. This ligament can be ruptured when excessive force passes through the joint and is usually associated with a twisting or “pivoting” injury. Sports more commonly associated with ACL injury include skiing, football, rugby and netball. Often the injury occurs in a non-contact or “off the ball” situation. A “popping” sensation is often described as this injury occurs followed by sudden pain and rapid swelling. The athlete is usually unable to play on. Following ACL injury it often takes several weeks for the swelling to settle and for the range of movement to return. Pain in the knee improves as the inflammation subsides. An ACL rupture is a very significant injury to the knee and is often associated with other internal derangement including meniscal tears, collateral ligament damage and damage to the chondral surfaces. Active patients often develop ongoing instability problems and giving-way symptoms that may lead to further damage inside the joint. Early referral to a knee specialist is recommended so that the knee can be fully assessed and appropriate treatment commenced.Treatment of ACL Injuries?
The correct management of ACL injuries varies and should be tailored for every patient. Treatment strategies depend upon patient age, activity, medical health, sporting & career aspirations as well as any concurrent injury within the knee.
Some patients are able to function very well with a deficient ACL ligament and can gain a “functionally stable” knee with strengthening and physiotherapy exercises. ACL reconstruction procedures may be indicated in more active people and “higher level” athletes who wish to return to sporting activities. Ongoing instability symptoms following ACL injury is generally an indication for surgical ACL reconstruction.
Collateral Ligament injuries
The collateral ligaments run on either side of the knee and prevent side to side instability. Occasionally these ligaments may become injured – either following a direct blow to one side of the knee or during a twisting type injury. Partial or incomplete tears to the collateral ligaments (particularly medially or inside part) are relatively common. The knee often becomes acutely painful and stiff with pain localised to the side of the joint.
Often these injuries can be managed with the help of a physiotherapist to help regain movement and function. With more severe or complete collateral ligament tears a knee brace may need to be worn for several weeks. Occasionally surgery may be needed to repair or reconstruct a badly torn collateral ligament.
Knee Arthritis
What is knee arthritis?
If large areas of protective cartilage are lost from the joint surface then arthritis develops. This is a common and painful condition that is often associated with stiffness, swelling and joint deformity (bowing of the legs). The commonest from of knee arthritis is osteoarthritis. This is often referred to as “wear and tear” arthritis and tends to occur in middle to older age. Some factors including knee injury, infections, family history and obesity may increase the chance of developing osteoarthritis or cause it to present at an earlier age.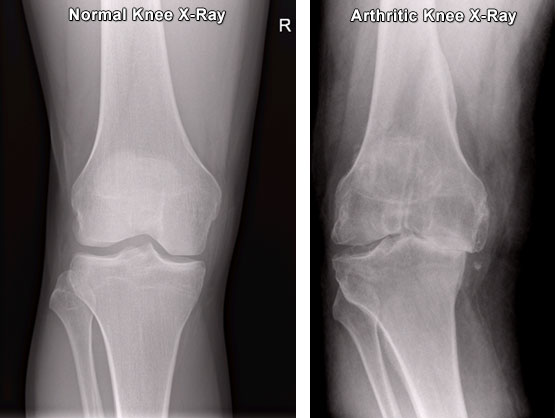
What is the treatment for knee arthritis?
In its early stages no treatment is usually needed and patients tend to put up with an occasional ache in the knee. As symptoms progress painkillers, braces and injections may all be helpful.
If non-surgical treatment is no longer effective then surgical intervention may be needed. Surgical options include joint realignment procedures to move forces away from the damaged area or partial and total knee replacements to resurface the joint.
What are the symptoms of knee arthritis?
Initial symptoms of knee arthritis are usually pain in the joint during or after activity and a moderate swelling. As the arthritis progresses the pain may also develop at rest or at night. Often the pain seems to be worse in the cold, wet weather and patients frequently describe a “toothache” sensation in the knee.
More advanced arthritis leads to increased stiffness in the knee and a reduced range of movement (initially an inability to fully straighten the knee). If the wear develops mostly on one side of the knee a “bow-legged” of “knocked-kneed” appearance may develop.
Get News & Updates
Stay in the loop with Northampton Orthopaedics with our latest news, events and advice.
What Patients Say

